COBRA
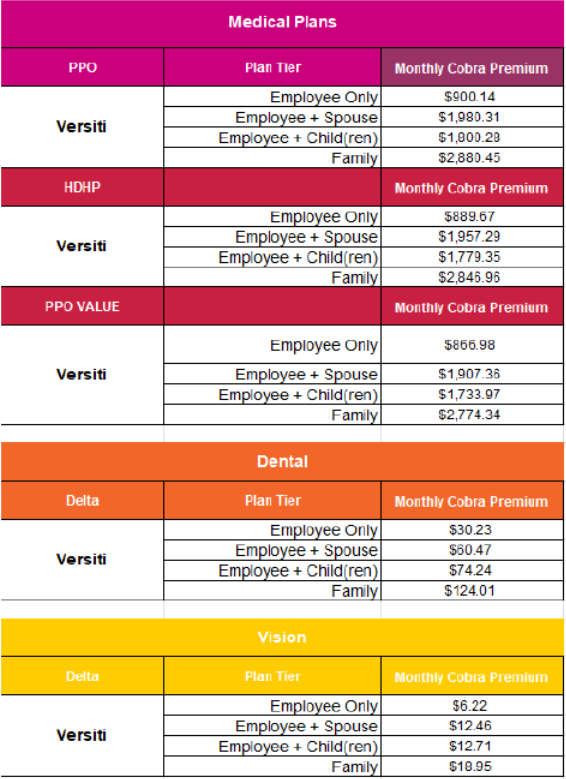
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a federal act that requires group health plans to provide a temporary continuation of group health coverage that otherwise might be terminated.
COBRA requires continuation coverage to be offered to covered employees, their spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain specific events.
In order to be entitled to elect COBRA continuation coverage, a qualifying event must occur; and you must be a qualified beneficiary for that event.. Examples of cobra qualifying events are:
〉 Termination of the employee’s employment for any reason other than gross misconduct
〉 Reduction in the number of hours of employment.
The following are qualified events for the spouse and dependent child of a covered employee if they cause the dependent to lose coverage:
〉 Termination of the covered employee’s employment for any reason other than gross misconduct;
〉 Reduction in the hours worked by the covered employee;
〉 Covered employee becomes entitled to Medicare;
〉 Divorce or legal separation of the spouse from the covered employee; or
〉 Death of the covered employee.
In addition to the above, the following is a qualifying event for a dependent child of a covered employee if it causes the child to lose coverage:
〉 Loss of dependent child status under the plan rules. Under the Patient Protection and Affordable Care Act, plans that offer coverage to children on their parents’ plan must make the coverage available until the adult child reaches the age of 26.
Source: United States Department of Labor